Ramatroban as a potential treatment for Sickle cell disease
Sickle Cell Disease
What is Sickle Cell Disease?
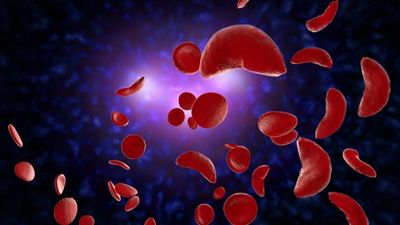
Sickle Cell Disease (SCD) is a genetic disease most prevalent in those of African descent caused by a single mutation in the HBB gene that leads to the production of hemoglobin sickle (HbS). Rather than maintaining their disc like shape when deoxygenated, red blood cells containing HbS hemoglobin undergo distortion, rigidity and structural damage that give them a sickle shape.
Vaso-occlusion
The sickle shape of red blood cells in SCD cause them to get trapped in small blood vessels, obstructing blood flow to organs. This leads to organ injury and failure. Obstruction of the small blood vessels by sickle red blood cells is referred to as vaso-occlusive disease which is often accompanied by pain crises.
Anti-Platelet and anti-inflammatory Agent

Adhesion Molecules
P-selectin is a well-known therapeutic target in SCD and is inhibited by crizanlizumab, a humanized monoclonal antibody targeting P-selectin (Ataga et al, NEJM, 2016). P-selectin along with other adhesion molecules including ICAM-1 and VCAM-1 promote the sticking of red blood cells to the walls of blood vessels leading to vaso-occlusion.
Thromboxane A2 (TxA2), an eicosanoid high in SCD (Foulon et al, Arterioscler Thromb, 1993), is a key mediator of platelet P-selectin expression, endothelial tissue factor expression and CD40L release, which all contribute to hypercoagulability and thrombosis in SCD. Conversely, TxA2 receptor (TPr) deletion significantly reduces the percentage of P-selective positive platelets (Matsui et al, Cancer Science, 2012); TPr antagonism also reduces endothelial and monocyte tissue factor expression after simulation with TNF-α or LPS, respectively (Bode et al, Vascular Pharmacology, 2014); and inhibition of TxA2 synthesis with low dose aspirin reduced plasma CD40L (Santilli et al, JACC, 2006). As a TPr antagonist, ramatroban is 100 times more potent than aspirin in inhibiting P-selectin expression (Kariyazono et al, Blood Coagul Fibrinolysis, 2004), and improves vascular responsiveness by also reducing endothelial surface expression of ICAM-1 and VCAM-1 (Ishizuka et al, Clin Exp Immunol, 1998), and potentially tissue factor and CD40L.
Hemolysis
Sickling of red blood cells causes them to become fragile and break down leading to release of heme. Cell free heme is normally catabolized by scavenging systems to be excreted in the bile, which are exhausted during states of excessive heme release including SCD. Oxidation of heme in the blood forms hemin which activates platelets by binding to the CLEC2 receptor (Bourne et al, Haematologica, 2020). Interestingly, CLEC2 induced platelet activation is dependent on TxA2 stimulation of the platelet TPr receptor. Ramatroban, at a dose 100-fold less than aspirin, inhibited platelet CLEC2 signaling induced by rhodocytin more potentially than aspirin (Badolia et al, JBC, 2017). Therefore, heme induced platelet activation is likely dependent on TxA2/TPr signaling which is blocked by ramatroban.
Thromboinflammation
TxA2 dependent CLEC2 signaling and platelet activation fuels the thrombinflammatory process of SCD characterized by platelet-neutrophil partnership, neutrophil activation, inflammasome activation and release of neutrophil extracellular traps (NETs). NETs are web-like chromatic structures containing DNA and histones that are normally geared to fight parasites and larger pathogens, contribute to formation of inflammatory blood clots and subsequent multiorgan failure in SCD (Chen et al, Blood, 2014). Myeloperoxidase is a marker of NET formation. Ramatroban was shown to reduce myeloperoxidase levels in the lungs, ileum and heart in a rat model of endotoxic shock (Altavilla et al, Pharmacol Res, 1994).
Analgesic

Mechanical Allodynia
Persistent allodynia (pain caused by a non-painful stimulus like light touch) and hyperalgesia (increased sensitivity to pain) can be part of the SCD pain experience. Mechanical allodynia is a type of allodynia caused by mechanical stimuli and is more prevalent among the SCD population than the general population (Molokie et al, J Pain, 2019).
The lipid mediators, prostaglandin D2 and thromboxane A2 contribute to neuropathic pain and mechanical allodynia via the DPr2 and the TPr receptors, respectively (Kanda et al, Glia, 2013 ; Pierre et al, J Invest Dermatol, 2017). Therefore, ramatroban has the potential to produce an analgesic effect to relieve SCD patients of their pain.
Depression and Anxiety
Depression and anxiety are common in patients with SCD and can worsen the quality of life for many. PGD2 via the DPr2 receptor plays a major role in depression symptoms. Pharmacological inhibition of DPr2 with ramatroban rescues abnormal social interaction and depression-related behavior in well-established animal models, including chronic corticosterone-, lipopolysaccharide-, and tumor-induced pathologically relevant depression models (Onaka et al, Behav Brain Res, 2015). Therefore, ramatroban has the potential to improve the quality of life for many SCD patients.
Pathophysiology of Sickle cell disease
Adapted from changeforscd.com